First DCD of liver in India: A new lease of life for patients’
Dr. Smriti Sharma Bhatia, Assistant Professor, Miranda House, University of Delhi-110007
Recently BLK hospital was in news for performing a liver transplantation of a 45-year-old patient after receiving the organ from a 60-year-old man post ‘cardiac death’. There are reported cases of donation after cardiac death (DCD) of kidney in India but there has been no case of DCD of liver recorded in the country before this. This is remarkable because liver transplantation is much more complex than kidney transplantation so it is much more challenging and special. Dadhichi Deh Dan Samiti had a chance to meet and interact with some of the members of the team at BLK hospital who performed this transplantation. Dr. Rajesh Kumar Pande, Director of BLK Center for Critical Care and Dr. Sanjay Singh Negi, Senior Consultant and Director, Department of HPB surgery and liver transplant at BLK Super Specialty Hospital, gave us valuable insights regarding liver transplantation after DCD.
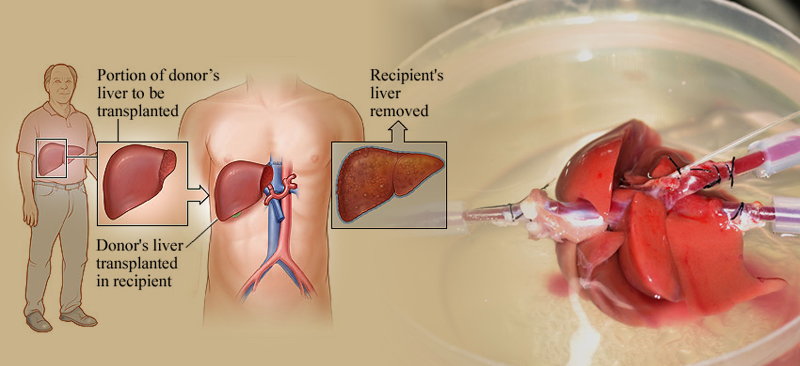
Recalling that day, Dr. Rajesh Kumar Pandey told us that the donor was a 60-year-old from Delhi, who was admitted to the intensive care unit and suffered cardiac arrest. The recipient is from Ghaziabad and was suffering from cirrhosis — chronic liver damage that leads to scarring and liver failure and had also suffered a stroke. The liver transplant took place in under four hours — a record. Explaining the process of Liver transplantation, Dr. Sanjay Singh Negi said that the new liver usually comes from either a brain-dead (cadaveric or deceased) donor or a willing living family donor. In India, it is usually a willing healthy living near relation who donates a part of his or her liver to the patient needing a liver transplant. This donor is usually an immediate family member- related emotionally to the patient. All living donors are subjected to several tests before transplant surgery. These include Blood tests, CT Scan, MRCP, Viral tests, Chest X-ray etc. These tests will ascertain the donor’s blood group compatibility with the recipient. These tests will also confirm that the part of the liver to be donated will be adequate for the recipient without risking a donor’s well-being. In addition to this, clearances are also needed for the donor from the Cardiologist, Pulmonologist and Gynecologist (if the donor is female). Besides making sure that the donor’s liver will work as it should, it is also important to establish that the donor has no other pre-existing disease. Transplantation involves a multi-disciplinary team approach wherein each case is put forward before a transplant board and discussed thread bare to ensure the best possible results.
Dr. Sanjay Singh Negi explained why DCD of liver is so challenging. He said thatusually organ transplants in the country are done from brain dead donors where the blood circulation is intact, cells are normally perfused and organs are still functioning at the cellular level. In case of DCD, blood supply to organ is briefly absent, causing the tissues to become starved of oxygen, a condition known as ischemia. Unlike kidneys, which have a long ‘warm ischemia time’ of about two hours, the challenge in liver transplant is a shorter ‘ischemia time’ of 30 minutes, which requires the graft to be re-perfused very fast.
 Dr. Rajesh Kumar Pande, Director of BLK Center for Critical Care
Dr. Rajesh Kumar Pande, Director of BLK Center for Critical Care
Dr. Pande explained that western countries have used DCD for a long time but somehow India has lagged behind due to societal reluctance and unfavorable perception of organ donation by families. According to him DCDwould be an effective way to reduce donor gaps in the country. Statistically speaking, in India, less than 5,000 kidney transplants are carried out annually against an approximateneed of over 175,000. Similarly, only 1,000 liver transplants are performed every year in a country where over 50,000 die due to end-stage liver disease.But the rate of organ donation is as low as 0.3 per million population (PMP).
 Dr. Sanjay Singh Negi, senior consultant and Director, Department of HPB surgery and liver transplant at BLK Super Specialty Hospital.
Dr. Sanjay Singh Negi, senior consultant and Director, Department of HPB surgery and liver transplant at BLK Super Specialty Hospital.
In this case, Doctors praised the readiness of the family to donate the liver. There are millions of people in our country who suffer from end stage Liver or Kidney Disease or any organ failure and await their death helplessly, in a desperate need of an organ transplant. They die painfully and in vain as there is seldom any solution to procure an organ for them and save their lives. The answer to such patients is Cadaver or Deceased Organ Donation. With advancement in medical sciences, human organ donation is fast developing into a major treatment protocol and is accepted as the best line of treatment for wide range of fatal diseases. However, despite the success rate of organ transplant surgeries, India still lags behind in the number of people coming forward for the cadaveric donation programme. Surprisingly though New Delhi has become the hub of organ transplant in Asia where more transplant surgeries are being conducted than any other city in the continent, still 99.9 per cent of all transplants are from their living family donors. This is contrary to the west, where more than 90 per cent of organs for transplants are from deceased donors. The successful implementation of organ donation hinges on the education of the masses and a proactive approach towards cadaveric organ donation, counselling of relatives for organ donation in the event of brain dead patients and a great co-ordination amongst hospitals is required to support this programme.
 On asking how the situation can be improved. Dr. Rajesh Pande said awareness and sensitization should be through media channels or by screening documentary films based on organ donation, expanding the group of doctors for certification of brain dead people and also by honouring cadaver donor families, etc. Both the Doctors agreed that it is very important that more and more people should be sensitized for organ donation and here the role of institutions like Dadhichi Deh Dan Samiti becomes very important.
On asking how the situation can be improved. Dr. Rajesh Pande said awareness and sensitization should be through media channels or by screening documentary films based on organ donation, expanding the group of doctors for certification of brain dead people and also by honouring cadaver donor families, etc. Both the Doctors agreed that it is very important that more and more people should be sensitized for organ donation and here the role of institutions like Dadhichi Deh Dan Samiti becomes very important.
On being asked how one can confirm the need for liver transplantation in a patient, the Doctors said that a team of doctors including liver transplant surgeons; hepatologists; a transplant coordinator and nurses among other health care professionals all working using a multi-disciplinary team approach. The transplant team begin by running a series of blood tests, an x ray, and other investigations to help decide the benefits from a transplant. • the patient’s heart, lungs, kidneys, and immune system are strong enough for surgery • the patient is mentally and emotionally ready for a transplant • the patient has a support system with family members or friends who can care before and after the transplant • the patient has the finances to cope with the long term care needed post transplantation We asked about the risks involved and were told that like any operation the Living Donor Hepatectomy carries a certain risk. The priority is always to reduce the risk to the donor. However despite all precautions, there is a 10 to 15% chance of a complication that would require treatment or prolong the hospital stay (normally a week or less). The most common complication is development of some fluid around the lung. Usually this requires no treatment other than breathing exercises but occasionally it may need to be drained under ultrasound guidance. Sometimes there may be leakage of bile from the cut surface of the liver or elsewhere. Usually this too does not require anything more than keeping the abdominal drain longer than usual. Sometimes it requires ultrasound guided drainage. Rarely temporary endoscopic stenting of the bile duct is required. Besides, like any operation, there is a small risk of death as a consequence of the operation. All over the world the donor mortality is in the region of 0.2% (just a little higher than the risk of mortality from driving a car on the streets of Delhi).
It was a pleasure to interact with these highly experienced and dedicated doctors and learn about DCD.
References
1. Interviews with Dr. Rajesh Kumar Pande and Dr. Sanjay Singh Negi
2. http://www.delhilivertransplant.com/

